What Is an Anal Abscess?
An anal abscess is a collection of pus around or in both the musculature and/or soft tissue of the anus. It can vary in size, duration, and location with 50% of abscesses developing into an anal fistula. Many people confuse these with hemorrhoids and a delay in diagnosis or a misdiagnosis can lead to significant complications, specifically if it’s STD related.
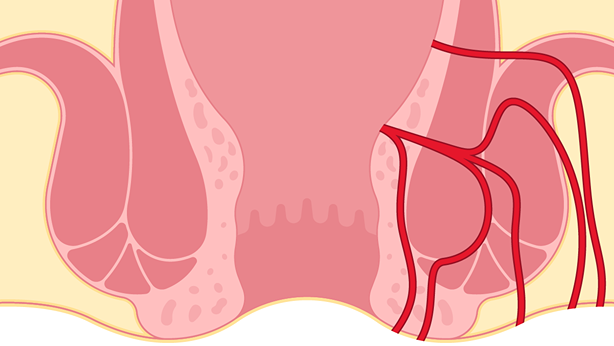
What Is an Anal Fistula?
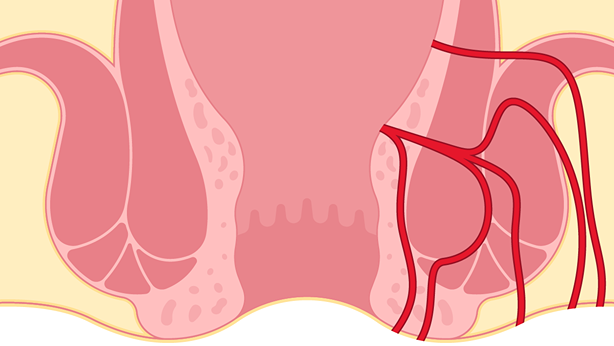
An anal fistula is an infected tunnel that develops between the muscular gland opening at the end of the anal canal and the skin near the anus. Anal fistulas need surgical correction, especially since it is probably limiting anal intercourse and/or anal play. It is quite common to have on and off periods of symptoms and these can range from simple to complex fistulas that develop. Depending on the situation, there are a multitude of procedures to eradicate the issue at hand. Anal anything is common in our bottoming world and fistulas are more and more evident as being limiting factors in anal play.
Anal Abscess & Fistula Causes
Anal abscesses are caused from a malfunctioning gland. The gland backs up and the fluid finds its way into the tissues to an exit near the anal opening. These are usually just the luck of the draw, but can occur from inflammatory bowel disease (IBD), as well as anal intercourse. Aggressive enema use from preparing for receptive anal intercourse, and STDs, can also be the culprit. Most anal fistulas are the result of an infection in an anal gland that initially presented itself as an abscess and subsequently spread to the skin.
Anal Abscess & Fistula Symptoms
Anal abscesses are generally associated with a throbbing pain that worsens when sitting. Discharge of pus or blood, constipation or pain with defecation, or anal skin irritation may also be present. An anal fistula is associated mostly with discharge and mild localized skin irritation, along with a hardened tract leading towards the anal opening. This sometimes looks like a large pimple on the exterior aspect of the anus or buttocks.
Anal Abscess & Fistula Diagnosis
Most anal abscesses/fistulas can be diagnosed by visual inspection. An anoscopy is usually deferred during the abscess period due to significant pain in region and drainage being required. Once a fistula develops, a full anoscopy may be performed in order to localize the internal connection and/or make sure no other pathology is associated.
Anal Abscess & Fistula Treatment at Bespoke Surgical
The appropriate initial regimen to treat an anal abscess/fistula consists of:
- Over-the-counter stool softeners, such as Colace, three times daily
- Over-the-counter fiber supplements, such as Metamucil
- Sitz baths, utilizing over-the-counter epsom salts
- Boosting your fiber intake with choices such as grains and whole-grain products, fruits, vegetables, legumes, nuts, and seeds
- Increasing your overall water intake to 8-12 ten ounce glasses per day
- Refraining from caffeinated beverages, as they tend to cause dehydration
- Keeping the anal area clean and dry. Wash gently with warm soapy water, and pat dry. Also, consider using something like an isotonic douching solution.
- Limiting the use of toilet paper, as wiping causes local inflammation. Please refrain from using baby wipes or medicated pads.
- Antibiotics for most anal abscesses, and sometimes for fistulas due to local inflammation
Anal pathology takes time to heal. You can imagine that every time it is attempting to improve, another local trauma/bowel movement occurs. Do not try to avoid having bowel movements, and try not to get frustrated as you work on the above regimen.
Anal Abscess & Fistula Surgical Treatment
Most anal abscesses require in-office drainage. Sometimes this may require monitored anesthesia care in an ambulatory setting. It is noted to be a 50% chance of complete eradication of the abscess after drainage and a 50% chance of development of an anal fistula. Strategic drainage of the abscess by professionals allows for improved location of fistula formation if this does occur. Generally speaking anal fistulas must be treated surgically, and are characterized as either simple or complex.
The vast majority of simple fistulas are treated with a fistulotomy, which involves cutting open the fistula in order for the tract to close. For complex fistulas, a technique commonly practiced involves ligation of the internal fistula tract (LIFT procedure) and removal of the remaining tract. If an abscess and tract is still present during the initial operative evaluation, a seton drain may be placed to allow maturation of this tract, followed by the LIFT procedure mentioned above or use of a cutting seton that is tightened in the office (pulling through the muscle, instead of transecting the muscle in the operating room, super important for our community since it is imperative to keep as much muscle in the game as possible.) Other anal abscess and fistula surgical options are surgical glue and placing an anal fistula plug in the fistula tract, but these do have limited successes.
We offer anal fistula surgery at our New York City location. To schedule your consultation, contact us today.
Fistulotomy Recovery
Depending on what surgical correction is implemented will determine the specific recovery. However, anal surgery, in general, is all similar in terms of timing. Usually, there is immediate constant pain and irritation in the first 2-3 days, followed by annoyances that happen more so during defecation. You may notice a small amount of blood draining from the opening of your fistula or pus discharge after fistula surgery. This is normal. You can put a gauze pad over the opening of the fistula to absorb the drainage if needed.
This can last for 1-2 weeks.
Finally, any anal work usually lasts for 6-8 weeks before one is fully recovered. As for bottoming or anal play, this will start roughly two months after surgery. After three months, you’ll be able to have anal sex after fistula surgery.
Now, just like we broke down the treatment by simple or complex fistulas, the recovery is similar. For simple fistulas, the procedure is just opening the fistula tract, which is now an open wound or similar to a fissure. This requires one to keep the area super clean and use the appropriate suppositories and lotions provided by the pharmacy for healing. Utilizing a bidet can also be supremely helpful in advancing the fistula and fistulotomy recovery process. During one’s subsequent office visits, we will place some chemicals to complete the healing process. It is not uncommon to drain some mucus or discharge until one sees us four weeks post-surgery. After the second (2-month) post-operative visit, a full internal evaluation is performed and if there are no issues, anal play with dilators will be initiated.
As for complex fistulas, this depends on what is performed and achieved. The ligation procedure is similar to that of simple fistulas and should be mirrored. The only deviation is if a drain, called a seton, is placed. This is done specifically if it is complex, with either an abscess still present or some technical reason to approach this in a two-staged procedure. Specifically in our gay community, it is done to spare any negative consequences to a procedure not warranted by others. With that said, it is a strategic placement to let everything settle down, allowing a staged procedure set you up for success. Remember: we need all the muscle we can get, specifically in the bottoming world. It is imperative one sees someone who has the knowledge to support all comers.
Prevention from Anal Abscess & Fistulas
Most of the time, this is a coin toss. It’s really the luck of the draw, so don’t stress too much about preventing fistulas. But in the bottoming world, less preparation is preferred. Anal douching can be a culprit because it irritates the anal glands. So when you do, remember: less force and less distention. What goes in, should come right back out. Also, STD prevention and/or early treatment is imperative since we do know these can increase one’s chances of having an anal abscess develop.
The other key component is to understand what an anal abscess or fistula is, and be seen by a surgeon with the knowledge to support our community. Sometimes the irritation one feels during anal play is actually the beginning of developing these issues. With early evaluation, a simple surgical correction can be initiated before the complexities develop. And lastly, remember to have a yearly anal external and internal evaluation by an experienced team.